Increase Your Census and Revenue by Leveraging Contingent Labor

Deirdre Baggot, partner, Oliver Wyman HLS
Lowered occupancy rates due to understaffing will cost the SNF industry billions of dollars in 2022. But facilities using contingent staff are showing positive margins.
Health care organizations often view part-time labor as a “necessary evil” due to the “premium” rate. But simply comparing hourly wages between part-time and full-time labor is misleading. Staffing shortages continue to drive occupancy declines in post-acute care facilities, but with organizational funding and reimbursement tied to patient volumes, every unoccupied bed or untreated episode represents a loss of revenue and a lowered ability to effectively invest and grow for the future.
Deirdre Baggot, a partner with the Oliver Wyman Health & Life Sciences Practice and David Coppins, co-founder and chief executive officer of IntelyCare, shared the findings of a new study examining the staffing crisis and the revenue implications of understaffing in a recent IAdvance Senior Care webinar, “The True Cost of Post-Acute Care Labor,” which was sponsored by IntelyCare. The two discussed how increasing staffing levels with contingent staff can increase revenue, improve full-time staff morale, and reduce turnover.
Survey Highlights
Oliver Wyman partnered with IntelyCare to assess labor dynamics and costs in the post-acute care space and provide health care executives with a comparative assessment of costs for full-time and contingent nursing staff. The organization maintained an independent, third-party perspective, while leveraging the insights of market experts and proprietary data sources for its research study, published in June 2022.
“We continue to see occupancy rates across all segments below COVID levels, anywhere from six to fourteen percent,” states Deirdre Baggot. “In the SNF industry, unrealized revenue in 2022 is estimated at over nineteen billion dollars due to understaffing. We found that the total cost of full-time nursing staff, including benefits, the cost of recruitment, and so forth, is 1.9 to 2.2 times the hourly wage for a full-time RN, LPN/LVN, and CNA. So, in terms of cost comparison, the true total cost for full-time nursing staff is roughly twice their normal base wage.”
Post-acute care nursing professionals are burned out, with many leaving their full-time jobs to work at staffing agencies. The survey found that 26 percent of nurses were considering leaving the profession entirely, with more than 60 percent who said they would not recommend nursing as a career. Fifty-nine percent of nursing professionals who left their jobs cited insufficient staffing as one of the reasons, and 99 percent ranked maintaining work-life balance as a top concern.

David Coppins, co-founder and chief executive officer, IntelyCare
“We can’t understate the current sentiment among nursing professionals,” adds David Coppins. “The workforce was pushed to a breaking point, and things are not returning to pre-COVID days. The nurses who have joined IntelyCare state that the number one reason they did so was because of the flexibility we offer them. The number two reason is work-life balance, and pay is number three.”
Emotional well-being and flexibility are clearly driving the decisions of many nursing professionals to make job changes. The survey data shows a correlation between staffing levels and perceived workload, and staff sense of well-being or burnout.
Addressing Capacity and Occupancy
While some executives consider closing beds because of staffing shortages, Baggot and Coppins make the case that leveraging a mixed workforce puts organizations in a better position long-term, and will restore occupancy rates to what they were pre-COVID.
“Lower occupancy equals unrealized revenue. The average skilled nursing facility is expected to lose between $2,300 to $6,000 a day due to staffing shortages. The facilities that are keeping their census low and staffing with their own employees are operating at a negative four to negative eight percent margin,” says Coppins. “The facilities that utilize contingent staff and increase their census are operating at a positive margin.”
Turning patients away can also negatively impact a facility’s relationship with hospitals and physicians.
The True Costs of Full-Time Labor
The survey data shows that on an hourly basis, the “fully loaded” cost of a new employee (RN, LPN/LVN or CNA) is 1.9 to 2.2 times the wage rate paid.
“The real wage for a full-time staff is not just the base hourly rate. Adding in benefits, overtime, payroll taxes, onboarding, and recruitment costs, additional contributions such as a 401(k) and paid time off, the true cost is about the same as for contingent staff,” Baggot states. “If the true cost of a CNA, for example, is $28 an hour and you’re paying $29 to $31 an hour for contingent staff, the real comparison becomes a $3 an hour difference. If not having enough staff is holding you back from taking on additional residents and increasing your census and your revenue, it may be a business decision that you need to revisit.”
Moreover, a national nursing shortage means that labor and benefits costs are not likely to decrease in the next several years, and recruitment costs, with sign-on and retention bonuses, are here to stay and likely to increase.
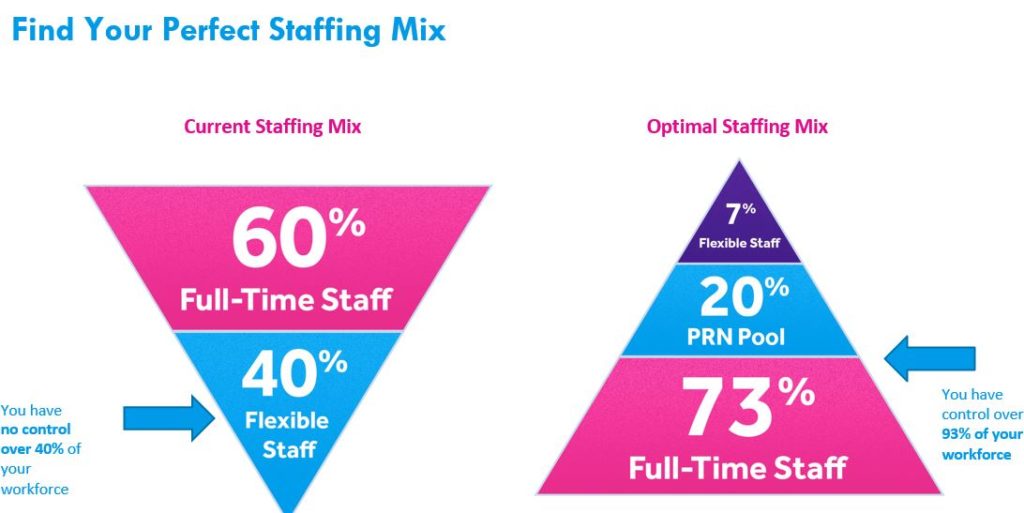
The Optimal Staffing Mix
Another factor to consider is reducing staff burnout.
“Hours worked have increased by up to 15 percent across the nursing workforce,” states Coppins. “Staff were already having a tough time keeping up with the demand and trying to keep a work-life balance. We hear so often that the workload is leading to people quitting, which reinforces a negative cycle since the rest of the group has to continue to work short-staffed.
“Working with contingent labor is a strategically smart way to get your census up, give your current workforce a break, and allow them to manage their work-life balance.”
Using technology to build their own PRN pool would give facilities the ability to meet workforce demands for flexibility. A mix of stable staff, a level of predictable contingent labor, and PRN pool can give the workforce the flexibility they seek in terms of scheduling.
Key Takeaways
- Burnout is driving out full-time staff, but there are correlations among improved staffing levels and reduced attrition/turnover.
- The SNF industry is losing billions in missed revenue due to understaffing.
- The total costs for full-time nursing professionals are nearly equal to the costs of contingent labor.
- Facilities should think of per diem platform providers and agencies as strategic partners that can be used to maximize revenue and ease the increasing burden on their staff.
Marlene Kurban is a freelance writer with more than 20 years of experience in nonprofit management and the behavioral health care field.

Marlene Kurban is a freelance writer with more than 20 years of experience in nonprofit management and the behavioral health care field.
Related Articles
Topics: Activities , Administration , Departments , Facility management , Featured Articles , Information Technology , Staffing , Surveys , Technology & IT











