Elder abuse: Zero tolerance
Legendary actor Mickey Rooney’s testimony during a Senate hearing last winter about alleged abuse suffered at the hands of a family member triggered national attention for victims of elder abuse, neglect and exploitation. Here was a well-dressed, alert 90-year-old, showing no signs of diminished cognizance, sharing a horrific experience of loss and betrayal. Media attention to Rooney’s case came on the heels of the late socialite Brooke Astor’s highly publicized story involving physical neglect and financial exploitation by her wealthy and well-respected son.
These two cases show that elder abuse isn’t restricted to those of modest means or limited education. And while domestic abuse and child abuse have attracted significant scrutiny over the past couple of decades, the scope of elder abuse has only recently gained attention as advocates push to bring this critical social issue to the public’s conscience.
Consider these figures from the National Center on Elder Abuse:
An estimated 1-2 million elders are abused annually.
Only one in 14 cases of elder abuse is reported.
Estimates of the frequency of elder abuse range from 2% to 10%.
A seminar on elder abuse presented at the Assisted Living Federation of America Conference & Expo in Orlando this past April focused on educating long-term care providers to identify abuse, train staff on how to respond if they suspect abuse and implement policies and procedures that should be in place to protect seniors.
Presenters Jean Sherman, EdD, RN, director, Center on Aging & Disabilities, University of Miami; and Anne Ellett, NP, MSN, senior vice president of Health Services, Silverado Senior Living, offered compelling case studies on elder abuse in long-term care and guidelines for providers to face this issue proactively to protect residents, staff and communities.
A DISTURBING CASE
“We [ALFA members] are stewards of the industry; we must step out as stewards of our residents,” asserted Ellett in her opening comments.
Ellett went on to share a disturbing case of elder abuse that occurred in 2007 in one of Silverado’s communities, which resulted in the death of a resident at the hands of a worker who had been named “employee of the month,” who was “friendly, engaging and communicative” and “very well liked among the staff.” An elderly male resident, found dead in his bed one day, had no outward signs of trauma but a criminal investigation of the case by detectives found internal trauma. Further sleuthing connected this caregiver to the crime and revealed that he was a dangerous sociopath. Ellett reported that this community had good systems, training, a culture of caring and a strong staffing model with RNs and LNs on staff 24/7. “We thought it [abuse] wouldn’t happen at Silverado but if it did we would know right away.”
We’ll return to the Silverado case later in this article.
SIGNS OF ABUSE
“Elder abuse has many faces because it is often passed down through generations,” said Sherman. “Elder abuse is a closely held family secret in many cases.”
Physical abuse indicators include unexplained welts, scratches, swelling, pain on touching and repeated falls; broken bones, often unset; multiple injuries in various stages of healing; and patterned injuries, like an imprint on the skin from a belt buckle. Signs of physical abuse include bruises or lacerations of varying ages; untreated decubitus ulcers (stage 3 or 4); ligature marks or finger or thumb imprints on wrists and ankles; and burns, including cigarette or scald burns.
Elder victim risk factors include cognitive impairment (e.g., dementia), poor health, social isolation and a shared living arrangement with a caregiver. Signs of neglect include poor hygiene, malnutrition, dehydration, skin abrasions, dirty toenails, soiled clothing and body odor. Signs of emotional abuse include apathy, depression, fearfulness and infantile or regressive behavior such as sucking, biting and rocking. Financial acts of exploitation commonly involve check theft, property transfers, embezzlement and property theft.
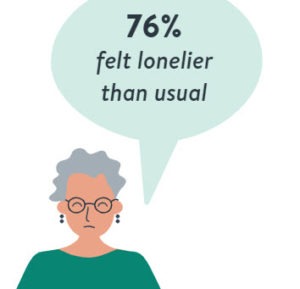
“My father used to beat me, my husband used to beat me, now my son beats me. I guess I’m used to it.” -76-year-old woman
ABUSER MOTIVATIONS
“The motivation of the abuser is primarily about power and control,” said Sherman. “The current economic climate hastens these situations. Perpetrators feel entitled.
“No one theory can explain abuse,” Sherman continued. “However, abusers harm older and/or vulnerable adults to exercise domination; they want to be feared, respected and ‘in charge’ and they feel entitled to use any means necessary to achieve their goals.”
Caregiver stress can lead to abuse. Predictors for caregiver stress include staff burnout, resident aggression, negative interaction between staff and residents and even negative interactions between residents-antagonism that might be encouraged by the abusive caregiver.
If a staffer has a history of substance abuse, a checkered employment history or legal problems, they are more inclined to take out their frustrations and negative feelings on those in their care. Also, an aggressive or unpleasant resident is more susceptible to neglect. And younger staff tend to have less empathy and are more inclined to neglect residents, said Sherman.
DOCUMENTATION, PREVENTION
It’s critical for providers to have good documentation of any case of abuse, said Sherman. Both written and photographic documentation are ideal. Report notations should provide no blank space between the note and one’s signature. Draw a straight line between the last word of the note and the signature. If a mistake is made in the notes, do not use correction fluid. Draw one straight line through it to allow it to be read. Write “error” above the mistake and sign it.
Sherman offered the following tips for prevention of elder abuse in long-term care:
carefully screen new hires for work history, criminal records, dependency, substance abuse;
educate all staff to look for abuse indicators and to report them;
educate residents about abuse-it is a crime;
encourage residents to report abuse by visitors, staff and other residents;
assure residents of no retribution for reporting; and
prominently post phone numbers for Adult Protective Services (APS) and the ombudsman.
Providers who fear losing their license for documenting abuse should put that notion to rest, said Sherman. In fact, she advised that one’s license would be at risk only when condoning, supporting or not reporting abuse. “We need to embrace and encourage reporting.” Sherman also expressed frustration over media exploitation of abuse cases. “They [media] should say they [caregivers] were on the ball and protected residents. They should look at you as heroes for reporting abusers and not as the bad guys.”
CHANGES AT SILVERADO
The case of elder abuse mentioned at the beginning of this article resulted in a murder conviction for the perpetrator. It triggered extensive organizational review at Silverado of practices and procedures including systems that “allow us to follow the early trail of suspicious activity,” said Silverado’s Ellett. “We talk about the possibility of abuse. We know it can happen. It is on the agenda of every meeting.”
Ellett went on to dissect the Silverado case. What put this resident at risk of abuse? As a resident with dementia, “he was a challenge to care for-not pleasant and he could be physically aggressive. He did not respond well to care and he was unable to articulate what was happening to him.” However, Ellett said, people with dementia can communicate distress through behavioral changes. Also, managers need to recognize caregiver fatigue. And, keep in mind, advised Ellet, “What came first: the resident’s ‘difficult’ behavior or perhaps their abuse?”
Other signs of potential abuse: Is there a culture of intimidation among caregivers? Are there staff cliques that do not support your corporate culture? Is there fear of reporting abuse?
ENGAGED LEADERS
An open, supportive, communicative culture can help foster an atmosphere of sharing and trust when it comes to recognizing and reporting cases of elder abuse. Community leaders must manage by being out on the floor-visible throughout the community on regular and irregular intervals, said Ellett. Management must acknowledge and talk about the possibility of abuse and neglect with staff and residents. Training is key. Abuse isn’t always so obvious. The use of restraints and overuse of sedation medication can signal abuse, for example. Staff should be regularly tested on procedures and engage in role-playing to recognize all potential signs of abuse and how to respond.
“We talk about the possibility of abuse. We know it can happen. It is on the agenda of every meeting.”
“We continue to educate ourselves and it has helped me-I always keep it [elder abuse] in the forefront of mind,” said Ellett. “We must have the moral courage to do the right thing.”
Web Resources
National Center on Elder Abuse
The National Center on Elder Abuse serves as a national resource center dedicated to the prevention of elder mistreatment. Go here for fact sheets, statistics, hotlines and tools to help your organization raise awareness of elder abuse in your community. www.ncea.aoa.gov
MedlinePlus
MedlinePlus is the National Institutes of Health’s website for patients and their families and friends. Go here for facts on elder abuse plus related links. www.nlm.nih.gov/medlineplus/elderabuse.html
Long-Term Living 2011 June;60(6):40-41

Patricia Sheehan was Editor in Chief of I Advance Senior Care / Long Term Living from 2010-2013. She is now manager, communications at Nestlé USA.
Related Articles
Topics: Articles , Regulatory Compliance