Back to the future through MDS
Next month we celebrate National Nurses Week and National Nursing Home Week. This makes it the perfect time to recognize what we do best, but for a different reason that is seldom recognized in the culture change movement.
There has been a tendency to see the Resident Assessment Instrument/Minimum Data Set as standing outside of the culture change movement. For years no one discussed the resident assessment process in concert with culture change, yet I viewed them as inseparable. The RAI process and MDS 3.0 is a step in the right direction, but let me begin by addressing the term “culture change.”
I don’t call this movement culture change and never have seen it that way, because how do we know what to change about the culture if we haven’t talked with the residents to identify their preferences? In nursing we have always done this through the nursing assessment process and individualized care planning. Thus, I have always felt this movement had it a little backwards in discussing culture without starting with resident “voice and choice” and assessment.\
 Using the presence of dining programs, neighborhoods and consistent assignment as the measure of an organization’s evolution toward culture change seems odd when by definition these interventions are based on someone’s assumption about what residents wanted as opposed to what they indicated they wanted through individualized care planning. An example of this comes to mind from my prior life.
Using the presence of dining programs, neighborhoods and consistent assignment as the measure of an organization’s evolution toward culture change seems odd when by definition these interventions are based on someone’s assumption about what residents wanted as opposed to what they indicated they wanted through individualized care planning. An example of this comes to mind from my prior life.
As a director of nursing, the ADON and I once decided it would be “less institutional” to wear colored uniforms and not wear nursing caps. This was at a time when nurses had just started wearing uniforms that were not white (wahoo!). It came to pass that the residents complained that they could not tell the nurses from the rest of the staff and wanted all nurses to again wear their caps. Neither the ADON nor I had a cap, as they were not a part of our nursing programs, so we flattened medication cups and pinned them in our hair for a few days.
My point is “less institutional” may not be a foregone conclusion. Making assumptions about residents’ preferences is dangerous business. When we simply ask residents, they surprise us more often than not. In fact, if you were to follow the culture change tenets, you might assume you were on track by wearing colored uniforms and no caps, but you might not be doing what the residents want at all. Perhaps we have evolved back to the future and it is time to put these assumptions aside and change the culture based on what residents indicate they want through the individualized assessment and care planning process.
Say it’s not true—the individualized assessment that my nursing instructors beat into my head is all it is cracked up to be in the end. We are back to the future because that individualized assessment should be the driver of changing facility operations so we address the preferences of the residents.
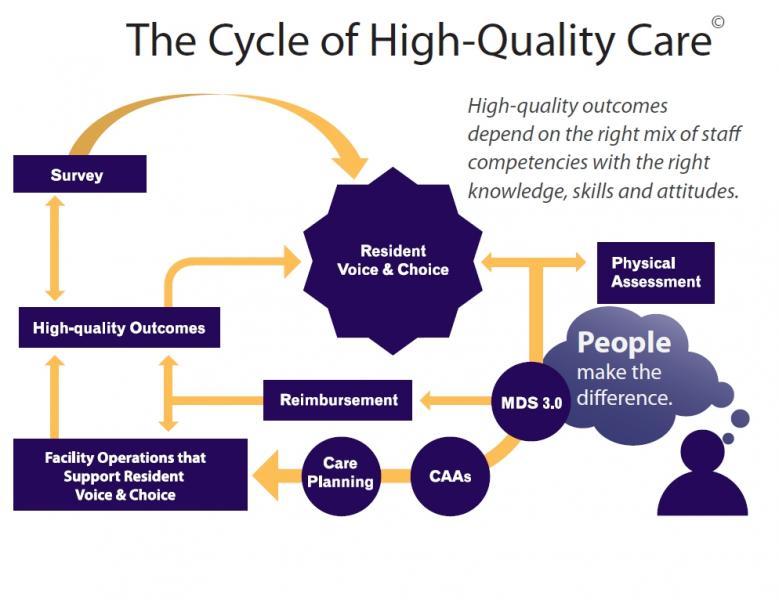
I recently developed a model of the “Cycle of High-Quality Life and Care” (see figure above), with the RAI/MDS process and resident voice/preferences at the center of the model, as the driver of facility operations. As you can see, this model assumes that high-quality outcomes will not happen without the right mix of staff competencies and the right knowledge skills and attitudes. Having that unique skills-set to build rapport with a resident so you are able to get clear direction from him or her in terms of preferences and choices is the core of our work as nurses and at the center of our core values.
This unique quality combined with expert assessment skills is the key to maneuvering that minefield between honoring a resident’s preferences and choices, physical assessment issues (nursing and medical needs), standards of practice, regulatory oversight and the highly litigious society we live in. It is time to recognize that nurses bring this unique knowledge to resident care, combined with an understanding of how to drive the residents’ preferences—and needs—while performing nursing and medical duties in a way that honors each resident’s preferences and choices.
So this National Nurses Day, celebrate your mission as a nurse by ensuring that the rights of residents who reside in nursing homes are protected. Do this through your unique skill sets as a nurse. Conduct expert nursing assessments that drive an understanding of what the resident wants most in terms of quality of life, balanced with quality of care throughout your community. After all, nursing assessment has always been about resident voice and choice.
Diane Carter, RN, MSN, CS, RAC-CT, C-NE, is President, CEO and Founder of the American Association of Nurse Assessment Coordination. She can be reached at Dcarter@aanac.org.
I Advance Senior Care is the industry-leading source for practical, in-depth, business-building, and resident care information for owners, executives, administrators, and directors of nursing at assisted living communities, skilled nursing facilities, post-acute facilities, and continuing care retirement communities. The I Advance Senior Care editorial team and industry experts provide market analysis, strategic direction, policy commentary, clinical best-practices, business management, and technology breakthroughs.
I Advance Senior Care is part of the Institute for the Advancement of Senior Care and published by Plain-English Health Care.
Related Articles
Topics: Articles , MDS/RAI , Medicare/Medicaid